 |
such a melancholic name.. such a malicious disease.. |

|

 |
WHAT IS CARDIAC TAMPONADE
|

CARDIAC TAMPONADE

Cardiac tamponade is a life-threatening condition caused by fluid under pressure around the heart. Fluid that collects in the pericardial sac (the tissue sac in which the heart lies) can develop enough pressure to prevent the heart from relaxing completely between beats. Usually, this fluid has accumulated rapidly, and the increase in pericardial pressure causes a sudden decrease in cardiac output.
 |
What's the Pericardial Space? |
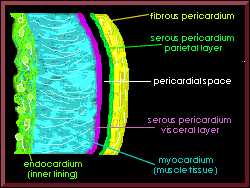
Pericardial Space
Above you see a dissection of the heart sac. On the left is the interior lining, on the right is the exterior lining. The pericardium is made up of all the layers right of the myocardial tissue. The pericardial space, also called the pericardial sac, normally holds about 25 ml of serous (serum-like) fluid. It is this small amount of fluid between the opposing layers of the heart wall that makes it possible for the heart to move easily without friction when it is contracting. As little as 100 ml of fluid in the pericardial space can cause problems. Remember.....
 | it is not so much the volume, but the rate of fluid accumulation that is responsible for the development ofacute life threatening conditions |

Too Much Fluid in Pericardial Space
The fluid can be blood, purulence, or effusion fluid (serum leaking out of blood vessels)...it doesn't matter. It just has to accumulate in that space surrounding the heart, causing increased pressure on the heart, so that the ventricles and atria cannot fill during diastole. With rapid accumulation of fluid, 100-200 cc may be enough to cause death. If the fluid accumulates slowly, the pericardium will expand, and perhaps 1 liter would be necessary to cause death.
 |
CAUSES OF CARDIAC TAMPONADE
|
THE MOST COMMON CAUSES ARE:
 |
* Hemopericardium
(blood accumulation in the pericardial space) usually from trauma or from
an aortic aneurysm that dissects (chest x-ray, 106K) into the pericardium.
Or iatrogenic (condition caused by medical treatment) like
anti-coagulation therapy, use of transvenous pacemaker, diagnostic
pericardiocentesis, CPR, cardiac catheterization or other invasive cardiac
procedures can also cause hemopericardium. |
 | * Neoplasm ("new growth" or
cancer) can cause rapid accumulation of serous or serosanguinous (mixture
of serous and blood) fluid in the pericardial space. 3. Pericarditis
(inflammation of the pericardium) from radiation therapy, infections, or
drug reactions such as hydralazine or procainamide can all result in
pericardial effusion that leads to tamponade. |
 | * Other Causes Of Cardiac Tamponade Include: Pericarditis, Acute Myocardial Infarction, Tuberculosis, Radiation Damage, Bacterial, Cardiomyopathy, Lupus, Or Dissecting Aortic Aneurysm. |
 |
PRESENTATION TABLE
|
 SIGNS AND |
 NURSING |
 HYMODYNAMIC |
 DIAGNOSTIC |
 POSSIBLE |
 -Dyspnea -Chest Pain -Weakness -Pulsus Paradoxus* -JVD -Cyanosis -Hepatomegaly -Cold Extremities -Feeling of fullness in chest -weakness -anxiety -rapid breathing -fainting -lightheadedness -chest pain radiating to the neck, shoulder, back or abdomen. It is sharp, stabbing worsened by deep breathing or coughing -abdominl swelling -skin color pale grey or blue -weak or absent pulse -drowsiness -low BP |
 -Diminished Heart Sounds (Sounds Muffled And Distant) -Pericardial Friction Rub -pallor -cyanosis -diaphoretic -tachycardia -narrowed pulse pressure -JVD |
 If the history and physical examination suggest cardiac tamponade, a pulsus paradoxus should be sought. In normal individuals, the height of the systolic arterial BP can decrease up to 10 mm Hg on normal inspiration. For this, the drop of systolic pressure on inspiration is greater than normal, since the interventricular septum bulges into the left ventricle as a result of the elevated right ventricular pressure. Simultaneously, pulmonary venous pressure falls more than usual because of negative intrathoracic pressure that is not matched by increased right heart stroke volume due to the Frank-Starling response. |
 ECHO -Echo Free Space between epicardium and the Pericardium that is hemodynamically significant. -RV Diastolic And/Or RA collapse in early diastole. -LV Diastolic And/Or LA Collapse in early diastole. -Dilated IVC can be noted. ECG -elevated ST segment if pericarditis is cause -electrical alternans-- alternating large and small QRS's -possible bradycardia or pulseless electrical activity -Ventricular dysrythmias Chest x-ray -widening mediastinum -cardiomegaly < |
 -Shock -Hypotension |

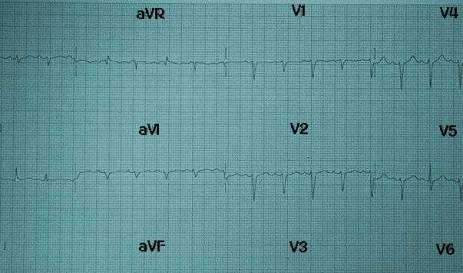
EKG of Patient with Cardiac Tamponade
The effectiveness of EKG studies in Cardiac Tamponade is highly debateable. Consider this study.....
"The Diagnosis of Pericardial Effusion and Cardiac Tamponade by 12-Lead ECGA Technology Assessment Mark J. Eisenberg, MD, MPH; Luisa Munoz de Romeral, MD; Paul A. Heidenreich, MD; Nelson B. Schiller, MD; and G. Thomas Evans, Jr., MD Objective:This study was designed to determine the diagnostic value of 12-lead ECG for pericardial effusion and cardiac tamponade.Design: Cross-sectional study.Setting: University hospital. Patients: Hospitalized patients with and without pericardial effusion and cardiac tamponade. Measurements and results: In a blinded manner, we reviewed 12-lead ECGs from 136 patients with echocardiographically diagnosed pericardial effusions (12 of whom had cardiac tamponade) and from 19 control subjects without effusions. We examined the diagnostic value of three ECG signs: low voltage, PR segment depression, and electrical alternans. We found that all three ECG signs were specific but not sensitive for pericardial effusion (specificity, 89 to 100%; sensitivity, 1 to 17%) and cardiac tamponade (specificity, 86 to 99%; sensitivity, 0 to 42%). None of the ECG signs were associated with pericardial effusions of all sizes, but low voltage was associated with large and moderate pericardial effusions (odds ratio=2.5; 95% confidence interval [CI]=0.9 to 6.5; p=0.06) and with cardiac tamponade (odds ratio=4.7; 95% CI=1.1 to 21.0; p=0.004). In contrast, PR segment depression was associated only with cardiac tamponade (odds ratio=2.0; 95% CI=1.0 to 4.0; p=0.05), while electrical alternans was not associated with either pericardial effusion or cardiac tamponade. Conclusions: Low voltage and PR segment depression are ECG signs that are suggestive, but not diagnostic, of pericardial effusion and cardiac tamponade. Because these ECG findings cannot reliably identify these conditions, we conclude that 12-lead ECG is poorly diagnostic of pericardial effusion and cardiac tamponade." |
 |
TREATMENT
|
Cardiac tamponade is an emergency condition that requires hospitalization. Treatment is aimed at saving the patient's life, improving heart function, and treating of the tamponade.
 |
Analgesics such as morphine, and diuretics such as furosemide (see furosemide - oral), may stabilize the condition until the fluid can be removed. | |
 |
Bedrest with the head slightly elevated minimizes the workload on the heart and may be recommended until the condition is stable. | |
 |
Oxygen reduces the workload on the heart by decreasing tissue demands for blood flow. | |
 |
The cause of the tamponade must be identified and treated. Treatment of the cause may include medications such as antibiotics, and surgical repair of injury. | |
 |
Removal of excess fluid from the sac (pericardiocentesis) may relieve symptoms and can be life-saving. | |
 |
Cutting and/or removal of part of the pericardium (surgical pericardiectomy) may be required if scarring is a cause of tamponade. | |
 |
Expectations (prognosis): Tamponade is life threatening if untreated. The outcome is often good if the condition is treated promptly, but tamponade may recur. |

BACK HOME NEXT