

 |

|

 |
WHAT IS COR PULMONALE |
Cor Pulmonale is defined as a complication of disorders that slow or block blood flow in the lungs, resulting from raised blood pressure in the lungs. A deadly form of Congestive Heart Failure, it creates enlargement or hypertrophy of the right ventricle in response to increased right ventricular afterload. Cor Pulmonale presents as right heart failure, which is defined by a sustained increase in right ventricular pressures combined with an inability to balance the cardiac output in response to exercise or other stimuli. Both sexes and all ages are effected by this devistating illness, but it is most common in men over 40.
 |
SYMPTOMS |
There are generally no symptoms in the early stages.
The most common presenting complaints of patients with cor pulmonale are:
 |
dyspnea on exertion |
 |
fatigue |
 |
Syncope and near syncope |
 |
chest pain |
 |
palpitations |
 |
leg edema |
 |
Distended neck veins |
 |
Bluish skin |
 | Enlarged liver and swollen abdomen |
 |
DIAGNOSIS |
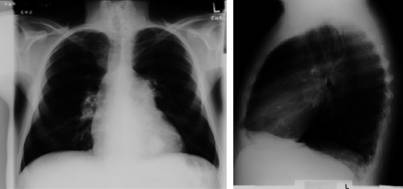
Lateral CXR Showing Cor Pulmonale
The chest x-ray may reveal right ventricular hypertrophy, manifest as filling of the retrocardiac space on the lateral film, and increased PA size.

EKG Indicating Cor Pulmonale
The ECG may be normal or show right atrial and ventricular enlargement as well as an R axis deviation. Supraventricular tachycardias are common.
Diagnosis is often expected based on clinical examination although findings may be subtle. Increasingly, the diagnosis of pulmonary hypertension is made with echocardiagraphy which demonstrates increased right ventricular size and wall thickness as well as evidence of ventricular interdependence (i.e. the septum moves with the right ventricle instead of the left). In the presence of tricuspid regurgitation (which is almost invariably present in right heart failure), pulmonary artery pressures can be estimated based on the velocity of the regurgitant jet. The diagnosis is confirmed with right heart catheterization which demonstrates elevated right atrial, ventricular and pulmonary artery pressures. Left atrial pressure is normal unless there is mitral stenosis or left ventricular failure. In addition, measurement of chamber oxygen saturations during right heart catheterization can be diagnostic for left to right shunts.
 |
TREATMENT |
PROBABLE OUTCOME--This condition is currently considered incurable. Many persons live 10 or 15 years after diagnosis, but disability will slowly increase. However, symptoms can be relieved or controlled. Lung transplants may be curative. Scientific research into causes and treatment continues, so there is hope for increasingly effective treatment and cure.
MEDICATIONS : These should include..
blood flow
ACTIVITY : There should be no restrictions. The patient should be as active as the condition allows, without overexerting. Rest between activities is vital.
DIET : Salt moderated
 |
TREATMENT OF UNDERLYING ETIOLOGY |
Anticoagulation or vena caval interruption are effective for thromboembolic disease. CPAP or tracheostomy can be used for obstructive sleep apnea, and correction of cardiac abnormalities is effective if the pulmonary vascular resistance is not substantially elevated.
 Afterload Reduction
Afterload ReductionMedical therapy is aimed primarily at decreasing right sided afterload. This can be done most effectively with oxygen via reversal of hypoxic pulmonary vasoconstriction. Two large studies of patients with chronic hypoxia (SaO2 less than 90%) and cor pulmonale secondary to COPD demonstrated marked survival benefits with long term oxygen therapy.
Vasodilating agents used in left heart failure are generally ineffective at decreasing right sided afterload as systemic hypotension is usually encountered before significant decreases in pulmonary vascular resistance are achieved. One clear exception to this is inhaled nitric oxide. The rapid metabolism of this drug prevents systemic vasodilation and hypotension. Furthermore its distribution solely to ventilated regions prevents the worsened hypoxemia due to impaired V/Q mismatching encountered with systemic vasodilators. Research in this field is active at present.
 Heart Failure
Heart FailurePeripheral edema and ascites due to right heart failure can be treated with diuretics. This must be done with care as decreased right ventricular filling can be associated with a catastrophic fall in cardiac output. Digoxin is not effective for treating right heart failure.
 Lung Transplantation
Lung TransplantationLung transplantaion should be considered for patients with end stage COPD, fibrotic lung diseases and primary pulmonary hypertension who have severe symptoms despite maximal medical therapy. Dramatic reversals in pulmonary hypertension and clinical symptoms are seen with this procedure, however, it carries the side effects of long term immunosuppression.